Available At
View Location
We provide diagnostic and therapeutic endoscopy services with wide spectrum.
The most common location for idiopathic anal fissure
90% are posterior, and 10% are anterior.
The most common symptoms of anal fissure
Tearing anal pain and bleeding with bowel movements.
The underlying pathophysiology of fissure in ano
Local trauma to the anal canal, internal anal sphincter dysfunction, and ischemia.
The differential diagnosis for anal fissure, especially if atypical in location?
Anorectal abscess, thrombosed hemorrhoid, inflammatory bowel disease, or malignancy.
Best diagnose anal fissure
By clinical history and visual inspection-not by digital examination or anoscopy (which serves only to turn a friendly patient into an irate one).
The nonoperative treatment options
High-fiber diet; stool-bulking agents; increased hydration; frequent, warm sitz baths; and topical agents containing anti-inflammatory agents, local anesthetics, and vasodilators (nitroglycerin).
The most common operation performed to treat intractable fissure in ano?
Fissurotomy with lateral internal anal sphincterotomy.
What is the most common cause of anorectal abscess?
Ninety percent result from cryptoglandular infection.
fistula in ano.
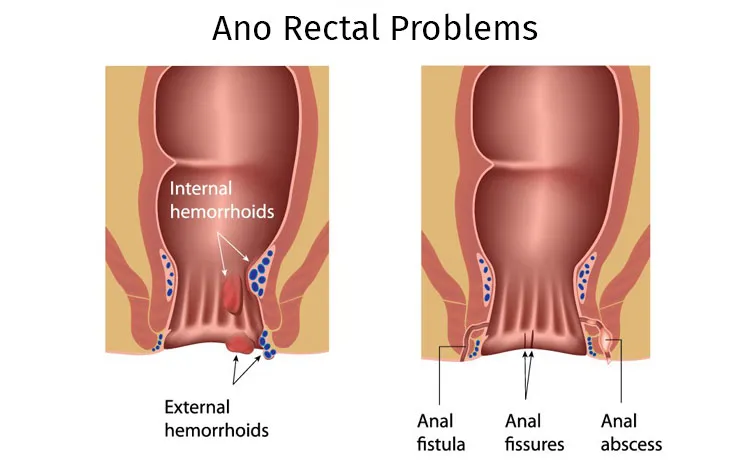
A fistula is an abnormal communication between any two epithelial-lined surfaces. The internal opening of the fistula in ano involves the anoderm at the dentate line, whereas the external orifice is located at the anal margin.
The incidence of fistula in ano after appropriate surgical incision and drainage of acute anorectal abscesses
50% Percent
The most important factor leading to the successful surgical eradication of anorectal abscesses or fistulas?
You must know anorectal anatomy, including the potential spaces of complications
The most important determinant of successful surgical treatment of fistula in ano?
Identification of the internal openings.
What is a seton?
A seton is a heavy suture placed through the fistulous tract that is then serially tightened, allowing slow, controlled transection of the sphincter. The associated fibrous reaction maintains sphincter integrity. Although associated pain is a limiting factor in its use, the technique can effectively change a high fistula into a low fistula with minimal risk of incontinence.
The management of anal fistula
Proper eradication of tract is the key factor by any means of management – like fistulotomy , fistulectomy, seton placement, laser fistulotomy , LIFT procedure and so on…
Normal function of hemorrhoidal tissues.
Hemorrhoids are cushions of vascular tissue that contribute to anal continence and protect the sphincter mechanism during defecation. Hemorrhoids are not veins, but sinusoids. Bleeding originates from presinusoidal arterioles, thus explaining the bright red arterial color.
The most common causes of problematichemorrhoids
Constipation, prolonged straining, pregnancy, and internal sphincter dysfunction.
The most important difference between internal and external hemorrhoids
Whereas internal hemorrhoids are located above the dentate line with visceral innervation, external hemorrhoids are located below the dentate line with somatic innervation. Ablation of internal hemorrhoids causes a pressure sensation with an urge to defecate, but a similar approach to external hemorrhoids causes excruciating pain.
The most common complaints associated with problematic internal hemorrhoids
Bleeding, mucus discharge, and prolapsing tissue.
The most common complaints associated with external hemorrhoids
Pain, inflammation, thrombosis, and difficulty with anal hygiene.
The treatment options for symptomatic internal hemorrhoids based on identifiable physical characteristics?
Yes. Treatment is based on the degree of prolapse:
Treatment options for haemorroids
Diet and stool bulking, rubber band ligation, injection sclerotherapy, cryotherapy, infrared photocoagulation, anal dilatation, or electrocautery.
Types Operative haemorrhoidectomy
The most common clinical presentation of a pilonidal sinus
Pain and swelling in the sacrococcygeal region, which typically are associated with a (sometimes several) chronic draining sinus tract.
The pilonidal disease acquired or congenital?
Acquired. Hair follicles in the midline sacrococcygeal area enlarge and become infected, resulting in an abscess.
Acute pilonidal abscess
Incision and drainage (like a fistula in ano, it is necessary to excise the whole tract)
The definitive therapy for pilonidal disease
Excision of the entire pilonidal cavity and associated sinus tracts down to the fascia with primary or delayed closure.
Theory explains the rarity of pilonidal disease after age 40 years
Changes in body habitus.