Available At
View Location
We provide diagnostic and therapeutic endoscopy services with wide spectrum.
Gallstones (45%), alcohol (35%), and other (20%).
Hyperlipidemia, hypercalcemia (hyperparathyroidism, multiple myeloma), iatrogenic factors (endoscopic retrograde cholangiopancreatography), drugs (didanosine, thiazide diuretics, H2 blockers, tetracycline, azathioprine), infections (mumps, coxsackievirus), pancreas divisum, and scorpion bites (favorite pimp question on rounds). Approximately 10% of cases are considered truly idiopathic.
Acute onset of severe epigastric pain that is boring in nature and often radiates to the back. Pain frequently is accompanied by nausea and vomiting.
The critical component of supportive therapy is fluid resuscitation to maintain urine output (place a Foley catheter). Nasogastric decompression in the presence of vomiting, pain medications, alcohol withdrawal prophylaxis, and avoidance of oral feeding until the patient clinically improves should also be done.
The inflammation and edema of acute pancreatitis may progress with subsequent devitalization of pancreatic and peripancreatic tissue. Pancreatic necrosis occurs in approximately 20% of acute episodes.
The presence and extent of necrosis are key determinants of the clinical course. Approximately 70% of patients with pancreatic necrosis develop infected pancreatic necrosis; infection accounts for 80% of all deaths from pancreatitis and is an absolute indication for surgery.
Dynamic computed tomography (CT) scans with contrast allow visualization and differentiation of healthy perfused parenchyma from patchy, poorly perfused necrotic tissue. CT-guided aspirate of the necrotic tissue should be sent for Gram stain and culture to determine the presence of infection.
Infected pancreatic necrosis is the only absolute indication for surgery. Open drainage is best accomplished via a bilateral subcostal incision, placement of the greater omentum over the transverse colon to prevent enteric fistulas, and removal of necrotic material from the lesser sac. The patient may require multiple trips to the operating room for repeated debridement; the abdomen is not formally closed until only viable tissue remains.
Patients who develop pancreatic pseudocysts typically present with persistent abdominal pain, nausea and vomiting, and an abdominal mass. One should wait 6-12 weeks for the pseudocyst to "mature" before undertaking operative or endoscopic drainage.
Attacks recur. Cholecystectomy is curative and is performed before patient discharge.
Attacks recur. Abstinence from alcohol should be encouraged because many patients develop chronic pancreatitis.
The classic syndrome consists of smoldering abdominal pain and evidence of pancreatic insufficiency. Histologically, chronic inflammation results in destruction of the functioning endocrine and exocrine pancreatic cells.
Alcohol abuse accounts for 75% of cases, but idiopathic chronic pancreatitis is also common in INDIA
The signs of pancreatic insufficiency
Insulin-dependent diabetes mellitus (found in up to 30% of patients) and steatorrhea (in 25%). Approximately 90% of the pancreas must be destroyed before diabetes develops
What is steatorrhea? How does one confirm the diagnosis?
Steatorrhea is soft, greasy, foul-smelling stools. A 72-hour fecal fat analysis may be done to confirm the diagnosis. The D-xylose test shows normal results, and the Schilling test is not sensitive for pancreatic insufficiency. Patients with steatorrhea are treated with a variable combination of low-fat diets, pancreatic enzymes, antacids, and cimetidine.
The complications of chronic pancreatitis?
Pancreatic pseudocyst, abscess, or fistula may occur. Obstruction of the biliary tree with resultant jaundice may be caused by areas of fibrosis. Malnutrition and narcotic addiction are more likely to coexist than actual complications of pancreatic insufficiency.
The indications for surgery in chronic pancreatitis
There are no steadfast rules. Relative indications include
The operative procedures are commonly performed in chronic pancreatitis
The frey procedure ( pancreatic head coring &lateral Rouxen-Y pancreaticojejunostomy) lays the Roux limb of bowel directly upon the "chain of lakes" duct to provide longitudinal head-to-tail drainage. Distal pancreatectomy may be used for isolated distal disease or retrograde drainage into a pancreaticojejunostomy. A modified Whipple operation (i.e., pancreaticoduodenectomy) can also remove a nonfunctioning but painful pancreas.
Hepatic abscesses are within the liver parenchyma:
The clinical features of hepatic abscesses are:
Diagnosis and management
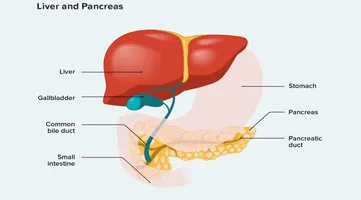
A diagnosis of hepatic abscess may be made by computed tomography (CT) or ultrasound scan, which is used to guide percutaneous drainage. For patients with a history of recent travel to endemic areas, serologic studies may be used to detect the presence of E. hystolitica antibodies. Percutaneous drainage is combined with systemic antibiotics. Occasionally surgical drainage is required for multiloculated abscesses containing debris.
The different groups of hepatic cysts are:
The general features of pancreatic cancer
There are about 30,000 new cases per year in the United States, and more than 29,000 deaths, so it is a highly lethal disease. In INDIA we don’t have proper registry, but cases are on rising trends. In most cases, histology is adenocarcinoma. About 80% arise in the head of the gland, and 20% arise in the body and tail. About 20% of patients have localized (potentially curable) disease at diagnosis; the remainder are inoperable either because of regional spread (portal vein, superior mesenteric artery) or widespread metastases (liver, peritoneum).
The presenting signs of pancreatic cancer
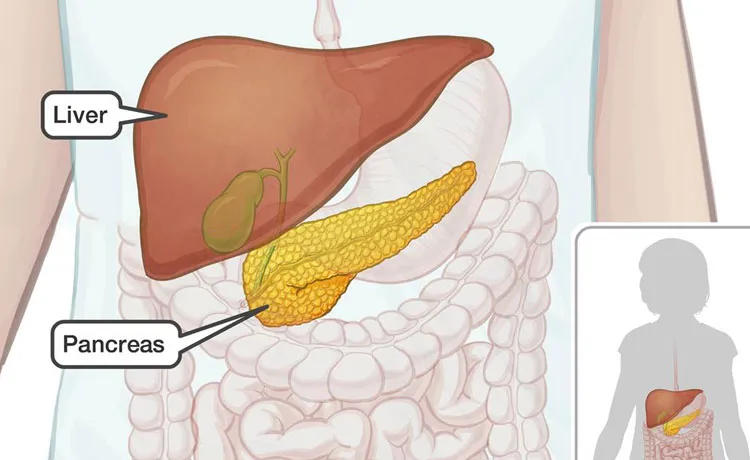
The pancreas is retroperitoneal and relatively insensate, and symptoms of disease are uncommon unless the pancreatic or biliary duct is obstructed or the process (pancreatitis, cancer) extends outside the gland. So many times it diagnosed late in course of disease.
A previously healthy old age person presents with pruritus, dark urine, and icteric sclerae after recent overseas travel. What is a reasonable differential diagnosis ?
The first step in evaluating in JAUNDICE.
The first step is liver function tests to determine the degree of jaundice and hepatic dysfunction. Then ultrasound is done to determine whether the cause is intrahepatic (normal bile ducts) or extrahepatic (dilated bile ducts). Ultrasound can detect stones in the gallbladder or common duct with about 95% accuracy. Thus, if a jaundiced patient has normal bile ducts on ultrasound, the problem is intrahepatic cholestasis, probably from hepatitis.
ERCP/ MRCP is best for determining intraluminal anatomy. CT scan provides other information, such as size of the tumor (if one is present), degree of regional spread (portal vein, lymph nodes), and presence or absence of liver metastases.
In this case, ultrasound, ERCP, and CT scan show dilated extrahepatic bile ducts, a mass in the head of the pancreas, and no obvious cause other than cancer. The tumor seems separate from the portal vein, and there are no liver metastases. Ideal management algorithm…..
If the patient is a poor operative risk, one should consider percutaneous or endoscopic ultrasound-guided fine-needle aspiration (FNA) to document cancer, if possible, and endoscopic stenting of the bile duct; surgery probably is not a good option. If the patient is a good operative risk, the next step is surgery. The clinical picture is accurate in at least 90% of cases, and FNA adds no useful information at this time. If no malignant tissue is obtained, surgery is still indicated because the needle may have missed the lesion, sampling only the pancreatitis that surrounds all such tumors.
This is a removal of the gallbladder, distal common duct, duodenum, and the portion of pancreas to the right of the portal vein-in essence, a proximal pancreatectomy. In some centers, it is also routine to remove the gastric antrum, with or without a vagotomy.
Distal pancreatectomy removes the portion of gland to the left of the portal vein, along with the spleen
Total pancreatectomy combines both procedures-again, with antrectomy in some centers.
With cure rates so low, why Whipple procedures is still main pillar of pancreas cancer treatment?
Unfortunately, this represents the only chance for cure. In addition, pancreatic resection-when carried out safely-probably offers the best long-term palliation in those destined to die of their disease. Finally, the outlook after pancreatic resection may improve in the future with preoperative chemoradiotherapy or newer forms of postoperative adjuvant therapy, so the future does have at least some hope.